The complications of spinal cord injury extend beyond the loss of motor function. There are a wide range of symptoms, which vary from case to case. Every year, approximately 250,000 to 500,000 people worldwide suffer from spinal cord injury. Motor vehicle accidents, a fall from height, and physical assaults are still the leading cause of spinal cord injury. Young males are most susceptible to traumatic spinal cord injury, especially from traffic crashes. However, elderly people, with preexisting spinal degenerative diseases, are at high risk of spinal cord injury due to minor trauma (e.g. falling).
Effects of different types of spinal cord injury
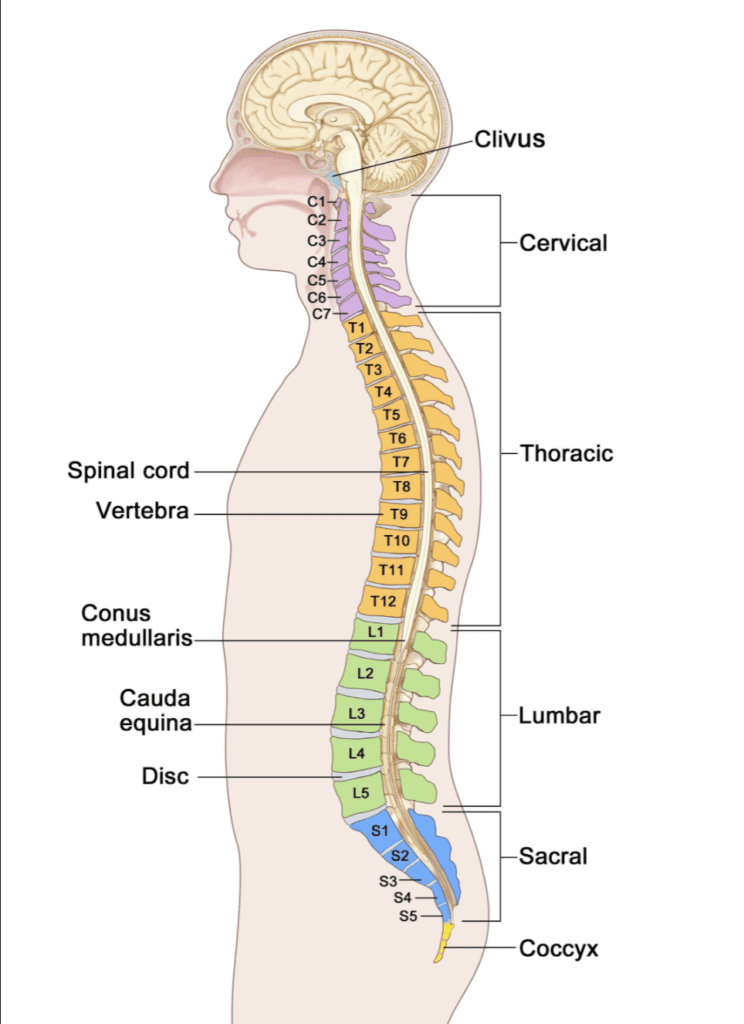
The higher the level of spinal cord injury, the more neurological impairment is found. For example, a patient with high cervical spinal cord injury will develop weakness of all extremities, called “tetraplegia”. They also have autonomic difficulties, such as respiratory insufficiency. A patient with thoracic spinal cord injury may have weakness of the lower extremities, known as “paraplegia”, but no impairment to the upper body. Patients with vertebral fractures below the lower tip of the spinal cord have an impact on the spinal nerve roots within the spinal canal. This causes damage to multiple spinal nerve roots, known as“cauda equina injury”. Patients with injury at this level always present with paraplegia, atrophy of the lower extremity muscles, and cannot voluntarily control urination and defecation.
Long-term, the effects of spinal cord injury include physical, psychological, and social facets. Psychologically, patients with spinal cord injury are vulnerable to mental illness, such as stress, anxiety, PTSD, or depression. In the social arena, disability can be challenging. People with spinal cord injury can struggle with the alteration to their lives and people with disability often experience prejudice and unequal opportunity.
Physical complications of spinal cord injury
With regard specifically to physical complications, the following are most common:
Weakness of the limbs
The spinal cord is the messenger system that transmits signals through the body, triggering movement. Spinal cord injury disrupts the signals between the brain and the limbs, therefore removing the brain’s ability to control them. This makes actions such as walking or using the arms impossible.
Low bone mass (osteoporosis) and fracture
In turn, the disuse of limbs is the major factor in the development of osteoporosis. Poor nutritional status, older age, and an elevated level of a stress hormone (cortisol) in the blood are also key factors of this condition. Patients with progressive loss of bone mass are at risk of impact fractures. The broken bones may occur spontaneously or due to impact, for example when the patient transfers from bed to wheelchair.
Frequent subtle infections
There are various infections to which SCI patients are more susceptible, the most dominant being urinary tract infections. After spinal cord injury, most patients lose bladder content and need an alternative urine management system. Commonly, these allow more bacteria to enter the bladder, leading to infection.
Respiratory insufficiency
Diaphragm paralysis is common in patients with high cervical spinal cord injury. This leads to respiratory depression – slower and less effective breathing or hypoventilation. Poor lung expansion leads to a higher risk of pneumonia because patients cannot cough effectively which impairs clearance of lung secretion.
Autonomic dysreflexia
This emergent condition is occasionally seen in patients with spinal cord injury at T6 level or above. It is more common in cases with cervical spinal cord injury and complete spinal cord lesions. Autonomic dysreflexia occurs as a result of a disturbance between functions of the autonomic nervous system in the body. A lack of sympathetic activity and overactivity of parasympathetic tone brings about many serious symptoms, such as headache, facial flushing, abnormal sweating, nose tightness and slow heartbeat (bradycardia). Common precipitating factors of autonomic dysreflexia include bladder or bowel distention.
Decreased blood pressure relating to the position (postural hypotension)
This adverse phenomenon is quite common in spinal cord injury patients, especially in injury of cervical or high thoracic spinal cord. The major symptom is a reduction of sympathetic activity resulting in dizziness, headache, sweating, and syncope.

Spasticity
This abnormal neurologic condition is very common following spinal cord injury. A lack of control signals from the brain to the muscles is the major cause of spasticity. Spasticity leads to functional impairment, postural disorder, joint or tendon contracture, pain, and pressure ulcers. However, spasticity also has advantageous effects, which you can read more about here.
Pain
A number of patients with spinal cord injury develop pain syndromes in variable periods after the injury. Disruption of the spinal cord tissue and damage of nerve cells may produce abnormal signals to the brain. This means the patients perceive that they have pain even though there is no connection between the brain and pain areas.
Pressure ulcers
This problem is very important and commonly found in spinal cord injury persons with immobilization. Patients’ lack of movement and repetitive injury of the skin covering the pressure areas, particularly over the bony prominences, lead to the development of deeper and deeper pressure ulcers. A large number of cases suffering from unhealed pressure ulcers require rehospitalization for the treatment. In some cases, the ulcers are difficult to manage because they involve the muscles, bone and sometimes lead to infection.
Fortunately, epidural stimulation treatment can offer some respite to patients experiencing these long term complications of spinal cord injury. The treatment improves both motor and autonomic functions, which can both directly and indirectly reduce these SCI effects. Whilst the treatment does not restore the patient’s condition to their pre-injury state, it can have a very positive impact on improving quality of life and physical comfort, and restoring some level of independence.







